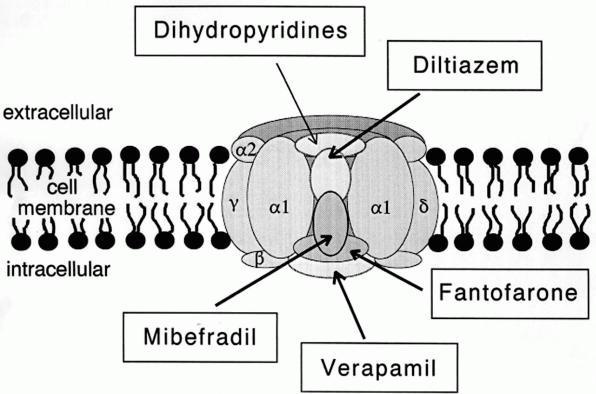
Calcium-channel blockers (CCBs) inhibit voltage-gated calcium channels, responsible for excitation-contraction coupling at skeletal, smooth, and cardiac muscle end-plates and sarcoplasmic reticulum, but also for conduction of the pace-maker signal in the heart.
INDICATIONS
- Hypertension
- Angina
Vascular smooth muscle
The non-dihydropyridines, diltiazem and verapamil, reduce coronary arteriole vascular resistance and increase coronary blood flow and myocardial oxygen supply, relieving angina symptoms. The dihydropyridines, amlodipine, felodipine, lercanidipine, nifedipine, and nimodipine, reduce peripheral vascular resistance (PVR) and blood pressure (BP) by relaxing arteriolar smooth muscle with minimal direct effect on the myocardial cells.
Myocardium and Cardiac conducting system (
The non-dihydropyridines, verapamil more than diltiazem, reduce cardiac inotropy and chronotropy.
Precautions
- myasthenia-like neuromuscular disease
- cardiogenic shock
- systolic heart failure (dihydropyridines may be used under specialist supervision)
- hepatic impairment: may require dose reduction
- elderly: start treatment at lower dose
Pregnancy (C): nifedipine is used to suppress preterm labour and for hypertension in pregnancy
Breastfeeding: limited data but diltiazem/nifedipine, nimodipine, and verapamil appear safe
- Angina may worsen on starting dihydropyridines, increasing dose, or stopping abruptly (reflex tachycardia and hypercontractility) although this is less likely with long-acting (or CR) dihydropyridines or use with beta-blockers.
- Aortic Stenosis — dihydropyridines may cause coronary hypoperfusion and systemic hypotension
Adverse effects
Common:
- nausea
- vasodilatory effect
- headache
- flushing
- dizziness
- hypotension
- peripheral oedema – dihydropyridines: due to redistribution of extracellular fluid rather than fluid retention – i.e. does not respond to diuretics but usually subside with continued treatment or dose reduction
Infrequent: palpitations, tachycardia, chest pain (dihydropyridines); orthostatic hypotension, abdominal pain, dyspepsia, diarrhoea, constipation (verapamil), gingival hyperplasia (usually reversible), polyuria (including nocturia), tinnitus, rash, itch
Rare: taste disturbance, LFT, extrapyramidal reactions, gynaecomastia, hypersensitivity reactions — Stevens-Johnson syndrome, exfoliative dermatitis, angioedema, vasculitis
Commercially available CCBs†
- Amlodipine: Norvasc, Nordip, Caduet (in combination with atorvastatin)
- Diltiazem: Cardizem, Vasocardol,
- Felodipine: Felodur ER, Plendil ER
- Lercanidipine: Lercadip, Zanidip
- Nifedipine: Adalat, Adefin, Nifehexal, Adalat Oros, Adefin, Adefin XL
- Verapamil: Isoptin, Isoptin SR, Isoptin CR, Anpec, Cordilox SR, Veracaps
†Australian market
 |
| diltiazem |
 |
| verapamil |
References
- Text: Australian Medicines Handbook, 2014
- Quotation: Wikipedia
- Images: Wikimedia Commons